Maternal mortality in India
From having maternal mortality rates well above the world average two decades ago, India has seen a sharp fall in the risk of death during pregnancy. Yet, regional disparities exist, and India is some distance from meeting international commitments
India has witnessed a steady decline in maternal mortality, driven by better maternal health and improved access to healthcare. Despite significant progress, regional disparities continue to exist, and India is still some distance away from meeting international commitments on reducing maternal mortality.
Current levels of maternal mortality in India
Maternal mortality refers to the death of a woman during pregnancy or within 42 days of its end, due to causes related to or aggravated by the pregnancy, excluding accidental or unrelated incidents. This definition, based on the World Health Organization (WHO), is also used by India[1].
Maternal deaths remain a significant cause of death in women, accounting for almost 7% of deaths of women in the 15-29 years age group as of 2020.
Maternal mortality data in India comes from the Sample Registration System (SRS), a large-scale continuous survey conducted by the Registrar General of India, designed to track births and deaths at the local level across India. The latest SRS report on maternal mortality, based on the data from about half a million births[2], covers the period from 2018 to 2020[3].
The most widely used indicator to understand how risky pregnancy and childbirth are in a region is the maternal mortality ratio (MMR), or the number of maternal deaths for every 100,000 live births. For every 100,000 live births in India in 2020, 97 women died of maternal causes. This translates to around 24,000 maternal deaths in one year alone[4].
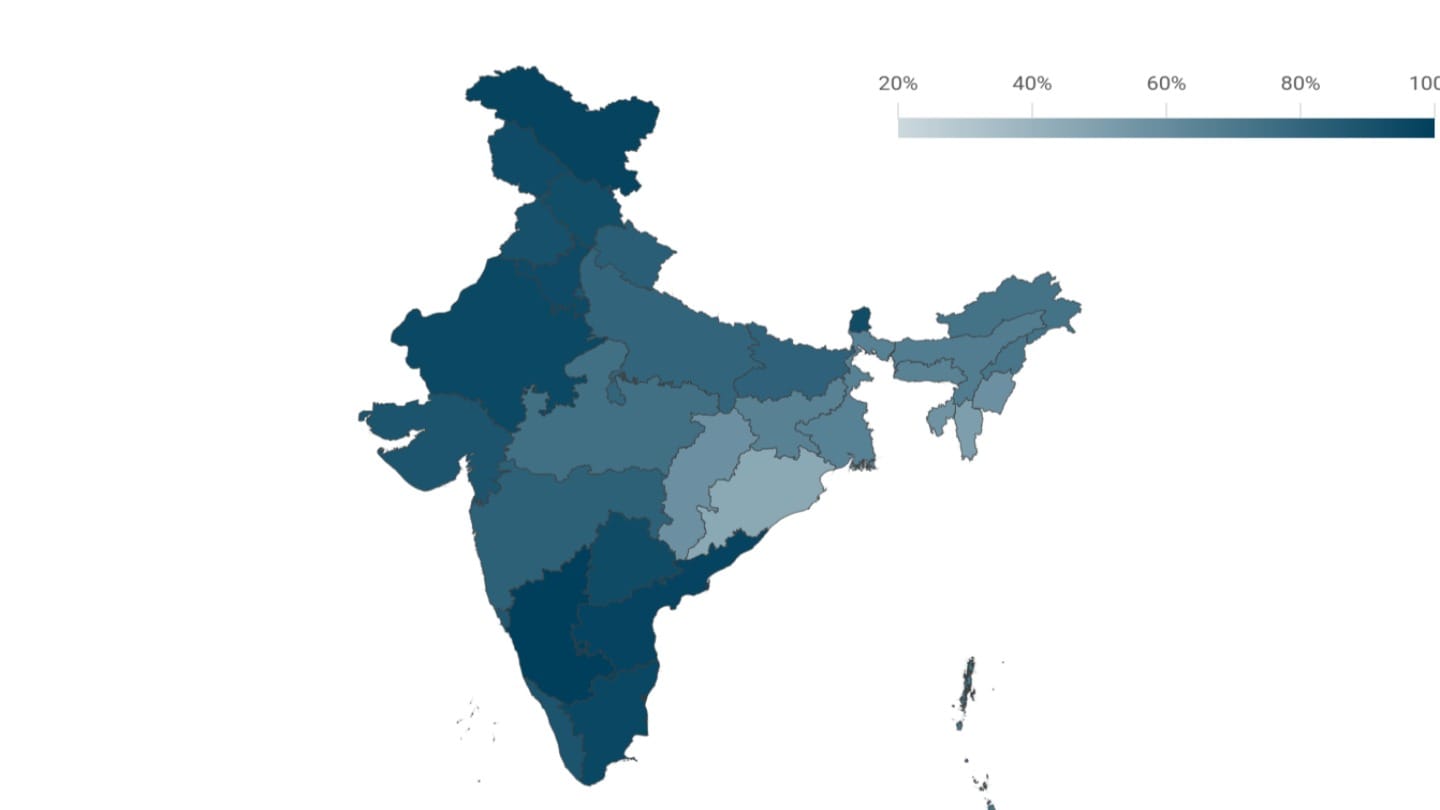
Maternal mortality levels in India vary widely across regions, with wealthier states generally having lower maternal mortality ratios. Kerala recorded the lowest MMR at 19 per 100,000 live births, which is even lower than the MMR in the United States, where it stands at 21[5]. States like Bihar, Madhya Pradesh, Rajasthan, Odisha, Uttar Pradesh and Assam have historically reported higher maternal mortality ratios, with Assam reporting India's highest maternal mortality ratio. These states face persistent challenges in healthcare access and systemic issues[6]. In contrast, southern states, with better healthcare systems, report lower maternal mortality ratios.
Progress over time
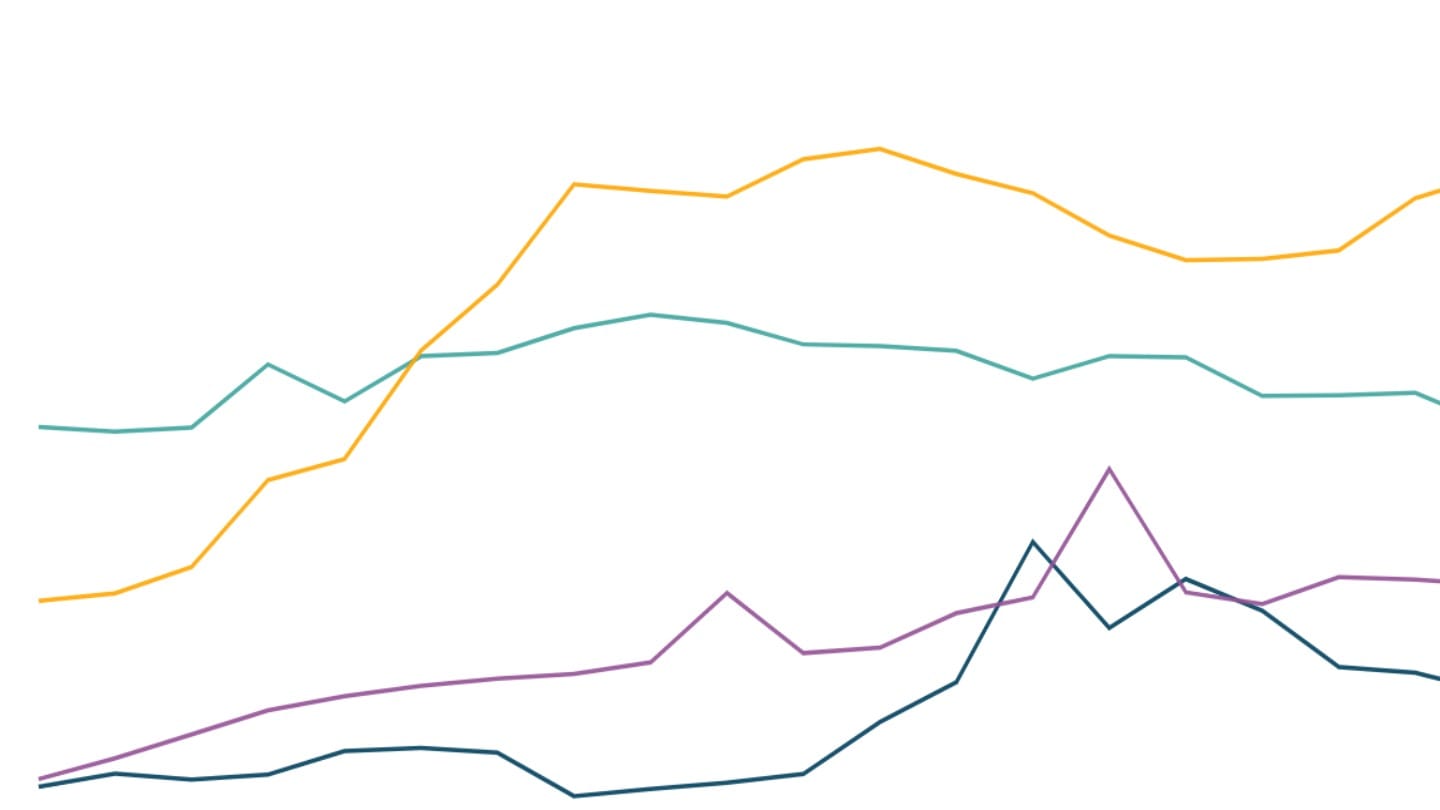
MMR in India has however significantly improved since the 1990s, driven by better access to healthcare, improved sanitation, enhanced nutrition, and broader social changes[7]. Maternal mortality in India stood at 398 per 100,000 live births in 1998, and by 2020, this number had decreased to a quarter of that figure, with 97 maternal deaths per 100,000 live births[8].
Globally, maternal mortality was 339 deaths per 100,000 live births in 2000, which was substantially lower than India's at the time[9]. By 2020, though, the global average stood at 223, more than double India's national MMR the same year. India's decline in MMR outpaced global trends over the last two decades.
Despite these advancements, however, India missed its 2015 commitment to reduce maternal mortality to 109 per 100,000 live births, with the actual figure standing at 130 in the 2014-16 survey[10]. India is also still some distance from the United Nations' Sustainable Development Goal (SDG) 3.1 of lowering maternal mortality to fewer than 70 deaths per 100,000 live births by 2030[11].
MMR is falling across all Indian states, and despite wide differences two decades ago, MMR numbers are beginning to converge between richer and poorer states.
Immediate causes of maternal death
Publicly available SRS data does not provide insight into the causes of maternal deaths. However the Million Death Study (MDS) conducted between 2007 and 2014 was a large survey within the SRS that used the "verbal autopsy" tool[12] to better understand causes of death. Using the MDS and other sources, a 2021 study[13] finds that the leading cause of maternal deaths in India is obstetric haemorrhage-excessive bleeding during pregnancy, childbirth, or soon after delivery. While this condition affects women across the country, it is especially severe in poorer regions like Bihar, Uttar Pradesh, and Uttarakhand. Between 2007 and 2014, more than half of maternal deaths in these areas were due to haemorrhage, with delayed diagnosis and insufficient treatment often proving fatal.
In wealthier states like Kerala, Maharashtra, and Tamil Nadu, pregnancy-related hypertensive disorders, such as pre-eclampsia and eclampsia, have emerged as significant threats. Pre-eclampsia refers to high blood pressure that develops after the 20th week of pregnancy, while eclampsia involves seizures in a woman already experiencing pre-eclampsia. In these states, nearly 2 of 10 maternal deaths were linked to these hypertensive complications, while haemorrhage remained a cause in 3 of 10 cases.
Another major factor contributing to maternal mortality in India is unsafe abortions, responsible for 5% of maternal deaths between 2007 and 2014.
In addition to the immediate medical causes of maternal mortality, several underlying factors make pregnant women more vulnerable to death during or after pregnancy.
Underlying factors affecting maternal mortality
Improved access to healthcare systems
Improving access to healthcare is a key factor in reducing maternal mortality. A study based on SRS 2001-03 data revealed that nearly half of maternal deaths occurred at home, with 13.8% happening in transit from home to health facility or vice versa[14].
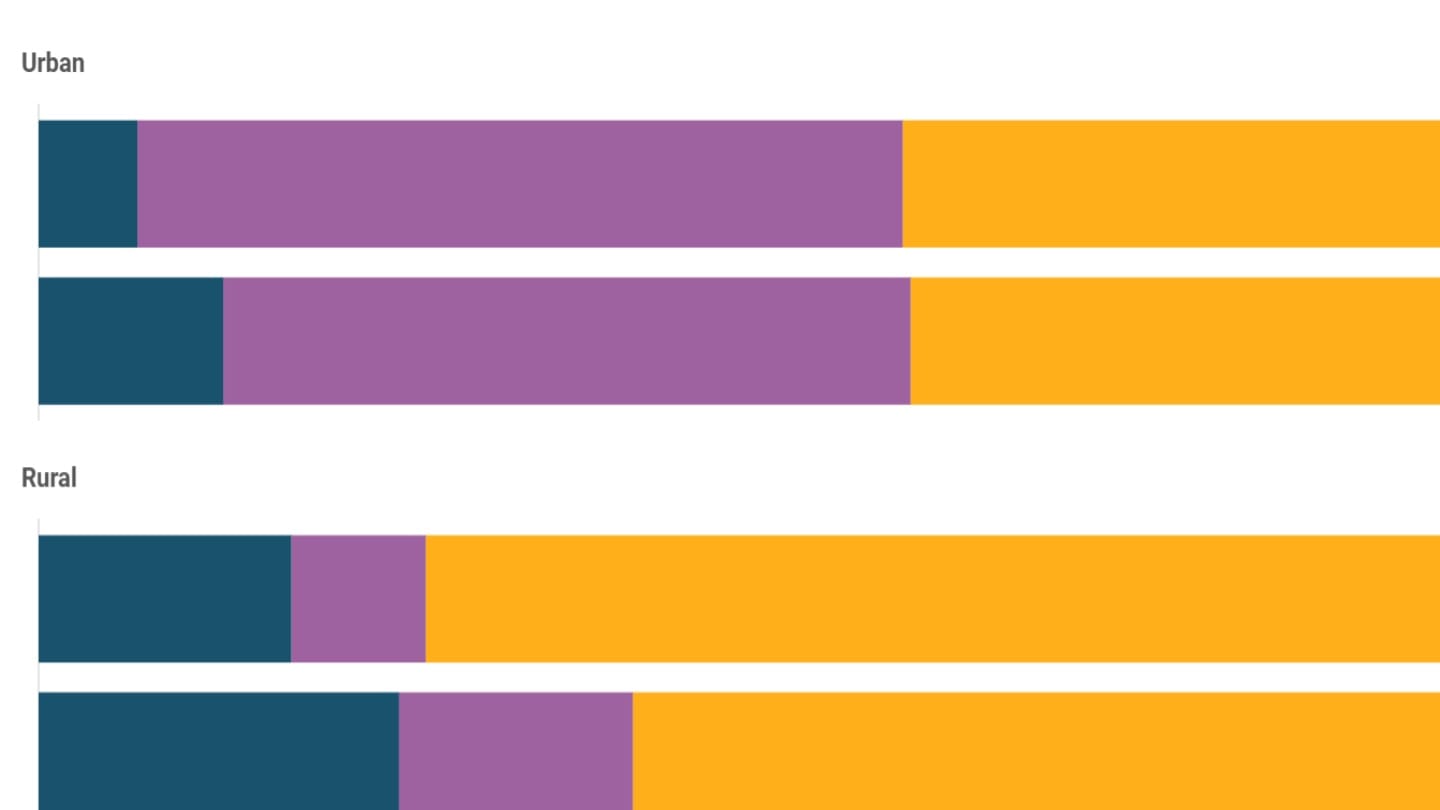
The number of institutional births has now increased significantly, lowering the risk of maternal mortality in India. In 1993, only a quarter of deliveries occurred in public or private hospitals, but by 2021, this had increased to 89%[15]. Yet, over a quarter of the poorest rural households continue to have home births.
Only 5 of 36 states - Arunachal Pradesh, Bihar, Jharkhand, Meghalaya, and Nagaland - still report over 1 in 5 deliveries happening at home[16].
Adequate healthcare during pregnancy is crucial for identifying complications early and providing necessary care, reducing risks before delivery[17]. Regular antenatal care (ANC) visits allow healthcare providers to monitor the mother's health, address potential issues, and ensure proper interventions when needed, thereby improving maternal and foetal outcomes[18]. The WHO recommends at least 4 ANC visits during pregnancy[19].
By 2021, 93% of pregnant women had had at least one ANC visit, and 60% had four or more. The proportion of women not receiving any ANC visit dropped from 38% in 1993 to just 6% in 2021. However, in the poorest rural households, 15% still do not receive ANC during pregnancy[20].
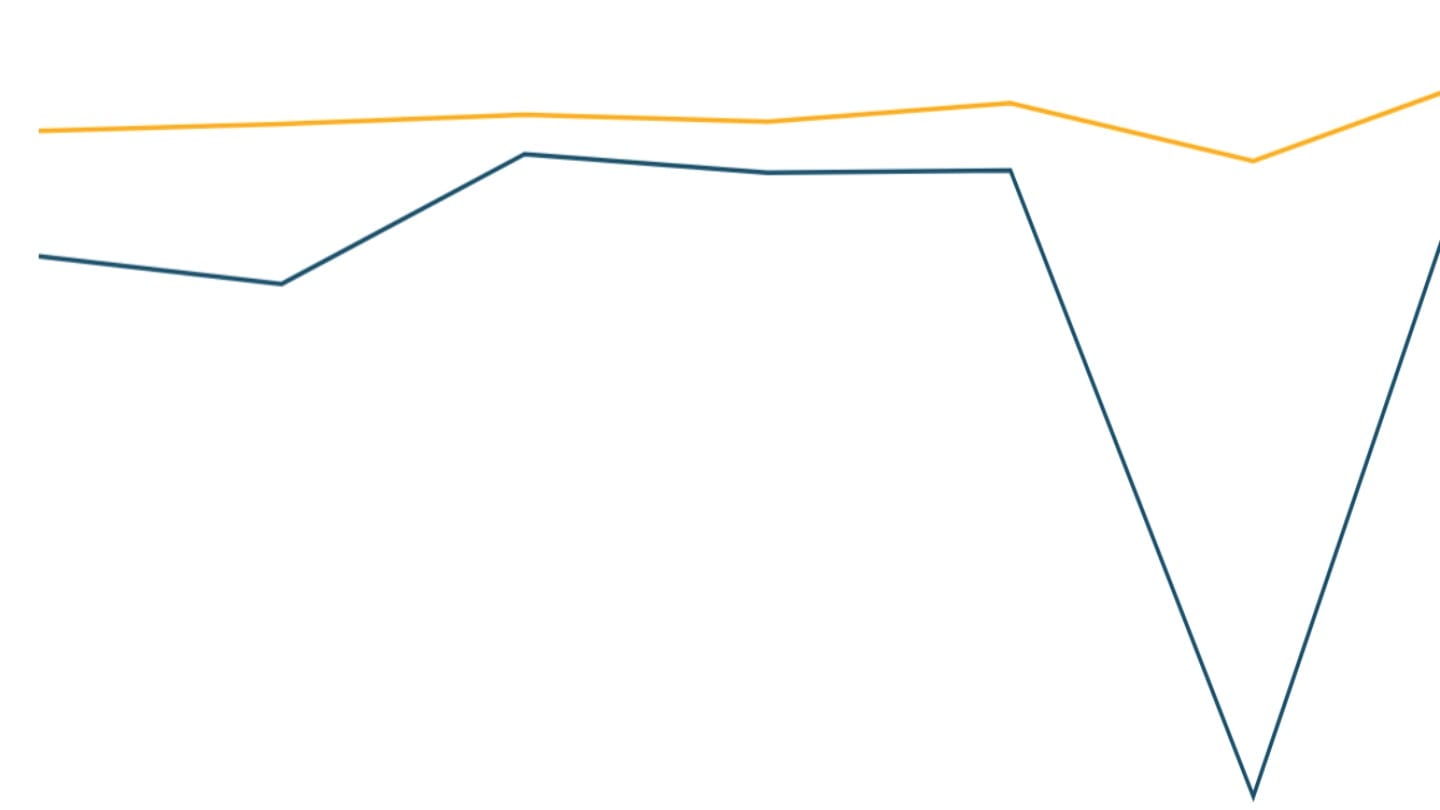
Mothers health
The age at which a woman has her first child is another factor in maternal mortality risk. Research shows that both age at marriage and maternal age at childbirth influence maternal health outcomes and affects the risk of maternal mortality[21]. Younger mothers also tend to utilise these services less frequently, which increases their health risks[22]. Over time, the median age at first birth in India has risen from 19 in 1992 to 21 in 2020, with the median age at first marriage also increasing from 16 to 19 during this period.
A mother's health plays a critical role in maternal mortality. Malnutrition and anaemia[23] can weaken a woman's ability to withstand childbirth complications, with severe anaemia particularly increasing the risk of obstetric haemorrhage[24]. Rates of anaemia among women in India remain high[25].
How is maternal mortality defined and measured?
Maternal mortality refers to the death of a woman during pregnancy or within 42 days of its end, due to causes related to the pregnancy, excluding accidental or unrelated incidents. This definition, based on the World Health Organization (WHO), is also used by India.
The Sample Registration System (SRS) estimates maternal mortality using a dual-record system where part-time enumerators record events such as births and deaths monthly, and full-time supervisors independently verify these details every six months[26]. In cases of death, a "post-death verbal autopsy" is conducted to identify the cause of death based on interviews with the deceased's relatives. Two independent physicians review the reports to assign a cause, with disagreements resolved by a third physician. This method allows reliable estimates by combining data from multiple sources and minimising discrepancies. Between 2018 and 2020, SRS surveyed approximately 24.6 million people. Using the crude birth rate from this period, the MMR dataset is based on about half a million live births[27].
Until 1997, maternal mortality estimates in India were based on smaller studies, which could not provide accurate data. Starting in 1997, the SRS introduced special surveys to determine maternal deaths, including retrospective methods in 1998. To increase reliability, the data was pooled over multiple years, providing more stable estimates for 1999-2001 and 2001-2003. Over time, verbal autopsies were improved to ensure better data collection.
From 2002, the SRS introduced RHIME (Representative, Resampled, Routine Household Interview of Mortality with Medical Evaluation), an enhanced verbal autopsy method. This approach involved structured forms, narrative collection, and independent re-sampling to ensure quality. Field staff were trained to collect symptoms and events leading to death without assigning a specific cause, improving data accuracy.
Research assistance: Nandlal Mishra
[1] World Health Organisation Global Health Observatory indicator metadata registry list
[2] The SRS MMR Bulletin pools data over three years due to the rarity of maternal mortality. In 2018, 2019, and 2020, the SRS covered a total population of 24.6 million overall. With crude birth rates of 19.8, 19.7, and 19.5 respectively, this equates to an estimated 483,726 total births during those years.
[3] There have been no new SRS rounds since 2020
[4] Based on an estimated 24.8 million live births in 2019, as reported by the UN statistical yearbook
[5] World Bank World Development Indicators
[6] The Maternal and Newborn Health India study identifies two clusters of states based on per capita income (PCI) and MMR to analyse the drivers of change. States such as Bihar, Madhya Pradesh, Rajasthan, Odisha, Uttar Pradesh, and Assam fall into the cluster with high MMR, low PCI, and limited access to healthcare systems. The study also finds that the density of health workers was lower in higher mortality states than lower mortality states.
[7] Maternal and Newborn Health India study
[8] SRS Special Bulletin on Maternal Mortality
[9] World Bank World Development Indicators
[10] Millenium Development Goal report, MoSPI
[11] SDG India Index report, NITI Aayog
[12] The 2021 study titled "Trends in maternal mortality in India over two decades in nationally representative surveys" utilised a modified WHO verbal autopsy tool, which includes a narrative in the local language provided by a family member. Maternal deaths were then classified using the International Classification of Diseases (ICD-10) after a review by trained medical professionals.
[13] The 2021 study titled "Trends in maternal mortality in India over two decades in nationally representative surveys" draws from multiple data sources to analyse maternal mortality in India and the key causes in addition to the MDS. These include the SRS Special Bulletins from 1997 to 2018, the National Family Health Surveys (NFHS) for 1998-1999, the Indian Institute of Health and Family Welfare survey, and WHO/UN model-based MMR estimates from 2000 to 2017.
[14] Maternal Mortality in India: Causes and Healthcare Service Use Based on a Nationally Representative Survey
[15] National Family Health Survey
[16] National Family Health Survey
[17] National Family Health Survey
[18] Positive experiences, key to antenatal care uptake and quality, WHO
[19] Global health Indicators, WHO
[20] National Family Health Survey
[21] Estimates and correlates of district-level maternal mortality ratio in India
[22] Social determinants of maternal health: a scoping review of factors influencing maternal mortality and maternal health service use in India
[23] A woman is considered anaemic if her haemoglobin levels fall below 12 g/dl, and is caused by poor nutrition, iron deficiency, and a lack of essential micronutrients like folic acid and vitamin B12
[24] Trends in maternal mortality in India over two decades in nationally representative surveys
[25] Anaemia in India, Data For India
[26] Maternal Mortality in India: 1997-2003 Trends, Causes and Risk Factors
[27] According to the SRS, the crude birth rates (CBR) for 2018, 2019, and 2020 were 19.8, 19.7, and 19.5, respectively